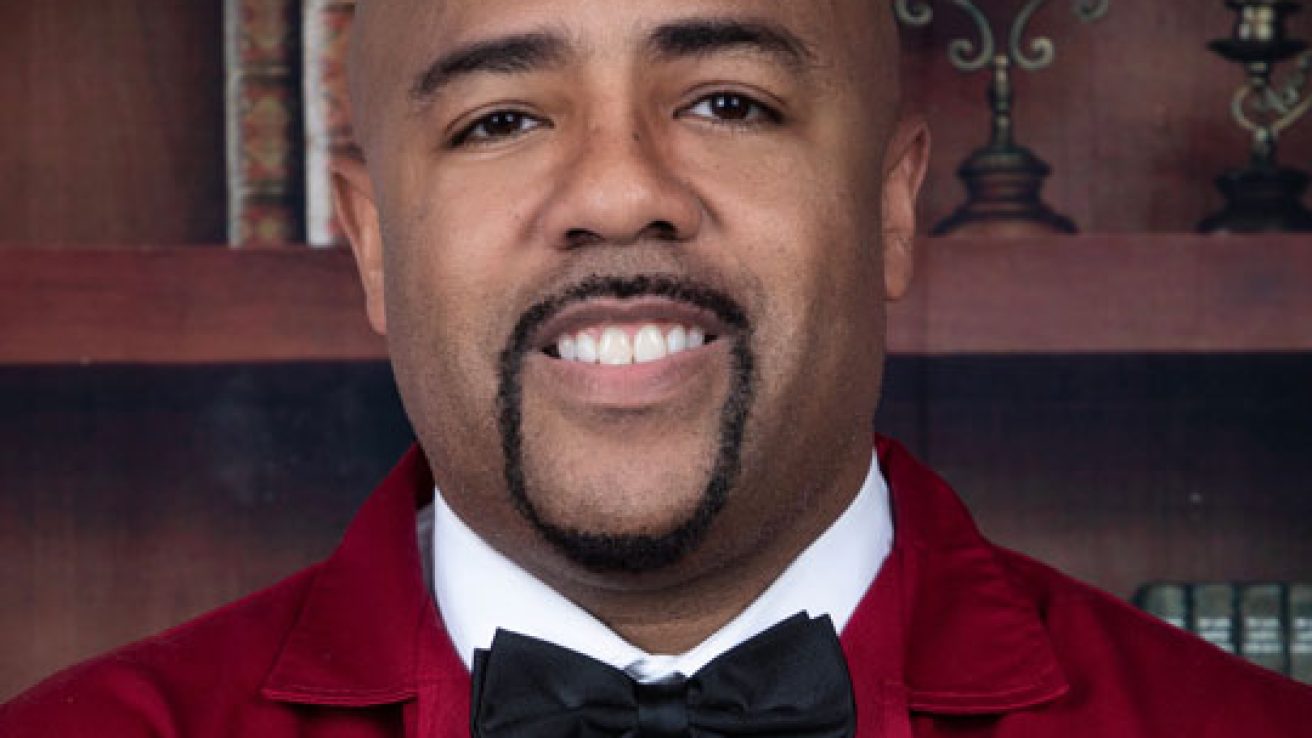
MD Newsline recently interviewed Dr. Michael Mcgee, Chairman for the Emergency Medicine Departments at Methodist Hospitals in Gary and Merrillville, Indiana and President and Chief Executive Officer (CE) of Premier Urgent Care and Occupational Health Center in Chicago, IL. Dr. McGee discussed clinical trial recruitment in the wake of COVID19 and the importance of recruiting more minorities in to clinical trials.
MD Newsline: How is recruiting for clinical trials during COVID different?
Dr. Mike McGee: Recruiting for clinical trials during the COVID Pandemic is obviously different for several reasons. First, patient volumes at medical centers and clinics are low because patients are limiting their face to face visits. Secondly, it’s very difficult to conduct seminars at facilities or on-site locations to increase awareness about clinical trials. Furthermore, it’s also very difficult to advertise or market valid trials because the current news media is fixated on the COVID Pandemic, as well as, the fast track of vaccines and studies that could be potentially harmful to patients, so the level of distrust is high.
Low accrual (enrolling) rates of patients jeopardize the ability of the researchers to assess the safety and effectiveness of new approaches to treatment care, wastes resources, and reduces the ability of the research to be translated into evidence-based practices. Under-enrollment of racial and ethnic minorities, particularly AAs, is an even greater challenge now despite a requirement by the National Institute of Health (NIH) that minorities be represented in clinical research.
MD Newsline: Why is it so difficult for health stakeholders to successfully recruit minority patients for clinical trials?
Dr. Mike McGee: In general, minorities have always been distrustful of any clinical trials due to years of systemic racism, but this has been overemphasized since the Syphilis study. A Systematic Review done in CANCER 2008;112(2):228-242 looked at barriers to recruiting underrepresented populations to cancer clinical trials. They found that mistrust in research and the medical system were the most common barriers to patients’ willingness to participate. Other well-known barriers were identified at the individual and systemic level as well as with interpersonal communication:
A patient’s major barrier is that they are not often aware of clinical trials and that they are eligible. An Audience Market Research Study by Boston Scientific states that 69% of Blacks reported that they have never even been asked to participate in a clinical trial. Also, some patients might be underinsured or might have co-morbidities that prevent enrollment.
Physicians might not be aware of available trials in communities most at risk. Some physicians might even perceive that their Black patients are mistrustful of physicians and medical institutions, so they never ask. Lastly, implicit bias may cause physicians to perceive their Black patients as less likely to comply with recommended treatment because it could negatively affect the timeline of the study. Family and friends should be included and could impact participation favorably or unfavorably.
Systemically, there are a limited number of trials nationally and regionally, especially in densely populated underserved areas with high prevalence of disease pathology. Minorities are usually in under-resourced hospitals, are under-insured and may have co-morbidities that make them ineligible.
Interpersonal: communication and transparency are very important and often lacking. Patients and Physicians in racially discordant clinical interactions should create a sense of common purpose (team approach), support, and understanding as ways to reduce bias and increase cooperation and trust.
MD Newsline: How can increasing minority participation in clinical trials benefit these communities?
Dr. Mike McGee: There are groundbreaking trials and new discoveries in effective medicines being produced every day that are not being utilized in vulnerable communities and populations that need them the most. Also, various minorities groups are affected differently by certain medicine due to genetic make-up. So different treatments can positively or negatively affect different ethnic groups differently. Also, the dose-dose interaction can be differently as well across groups.
An example is with cancer research. ProPublica and Stat reported this year (www.propublica.org) that in trials for 24 of the 31 cancer drugs approved in the past 3 years, less than 5% of the subjects were AA. This is concerning because AAs account for 13% of the nation’s population but have the highest death rates and shortest survival rates (www.cancer.org) of any group in the US for most cancers.
MD Newsline: Can you tell us about the clinical study you are recruiting for?
Dr. Mike McGee: Nitric Oxide (NO) has been safely used clinically for many decades. It is the loss of NO production that puts African Americans at greater risk of COVID infection complications and greater risk of hospitalization need for ventilation and death. Nitric Oxide Innovations (NOI), LLC has received IRB approval (www.clinicaltrials.gov) – NCT04601077 as a part of the Coronavirus Treatment Acceleration Program (CTAP) from the US Federal Drug Administration (FDA) to begin an outpatient clinical study testing the safety and efficacy of its new drug. NOviricid is the first oral Nitric Oxide (NO) generating drug to be clinically tested to treat African Americans diagnosed with COVID – 19. This is the first and only COVID-19 study that specifically addresses this particular health disparity in African Americans – one of the most affected, high risk populations of the virus.
Dr. Nathan S. Bryan, Founder and CEO of NOI stated, “Everything we learned about COVID 19 over the past 10 months reveals that diminished nitric oxide production in patients is what is thought to be responsible for the increased risk of infection and rapid disease progression. Restoration of Nitric Oxide via Noviricid 30 mg lozenge promises an easily administered, safe, affordable, and effective treatment.”
Patients (50y old – 85y old) who are African American and recently diagnosed with COVID 19 within 72 hours are eligible, if they have at least 1 of the following pre-existing conditions: High blood pressure, diabetes, smoker for more than 4 years, heart disease (heart attack or coronary artery disease), Obesity, or COPD. If the patient qualifies, they will receive a free pulse oximeter to measure their oxygen level, a blood pressure monitor, and $100 cash for completing the study. They will also be followed by the Institute of Clinical Therapeutics via Telemedicine for 30 days an observed for outcomes.
Learn more about the COVID19 clinical trial Dr. McGee is recruiting for : Clinical Study Begins for the First Oral Systemic Nitric Oxide Based Therapeutic for African Americans with COVID-19 and visit Premier Urgent Care today.