![]() Medically reviewed by Dr. Kimberly Langdon Cull, M.D. on July 25, 2023
Medically reviewed by Dr. Kimberly Langdon Cull, M.D. on July 25, 2023
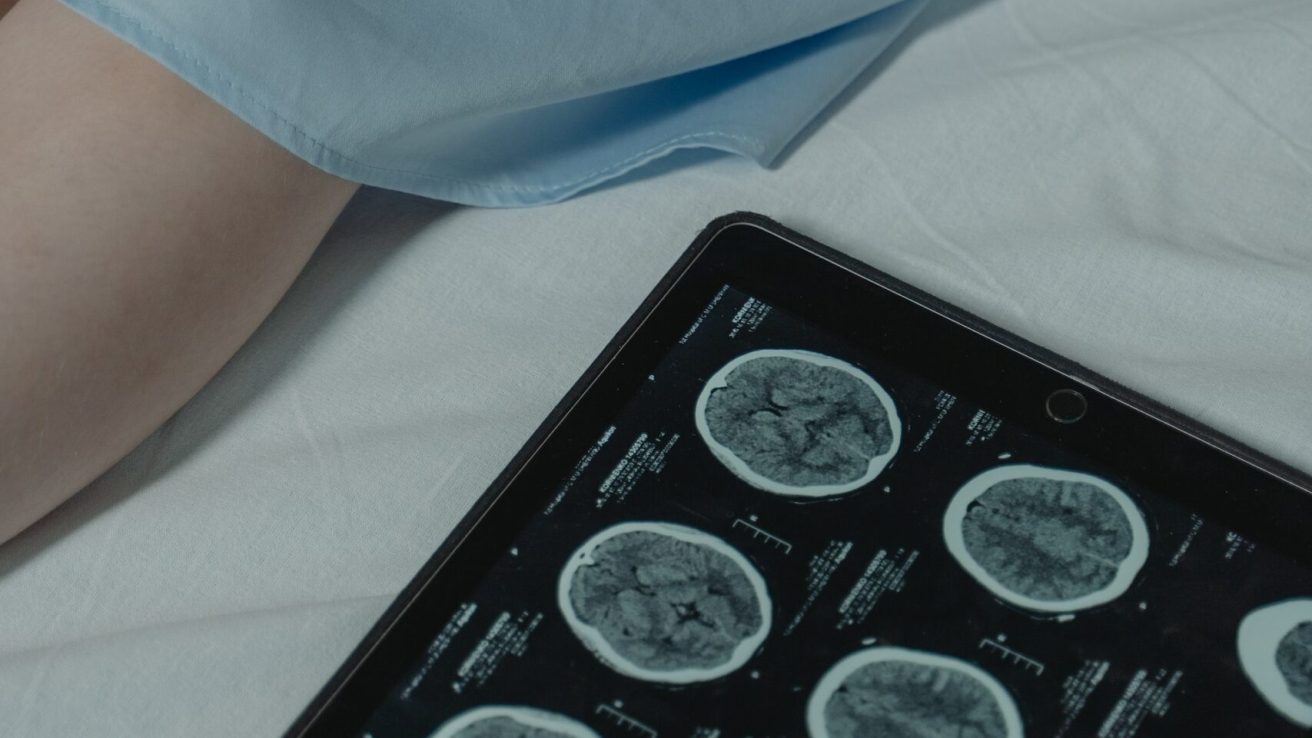
In midlife women, vasomotor symptoms during sleep are associated with increased white matter hyperintensity volume. Such brain health markers can aid in the identification of menopausal women who may require early prevention and intervention measures.
Vasomotor symptoms (VMS) in menopause tend to be linked to poor cardiovascular health and cognition. There is limited data pertaining to the association between VMS and brain health markers, including white matter hyperintensities.
This study investigated the association between physiologically assessed VMS and increased white matter hyperintensity volume (WMHV), an indicator of small vessel damage, in midlife women. The findings are published in the journal Neurology.
Study Characteristics
Based on the eligibility criteria, 274 women with an average age of 59 years were enrolled, out of whom 239 underwent neuroimaging. Approximately five physiologically assessed VMS were observed in the participants over a period of 24 hours.
Vasomotor Symptoms and Whole Brain White Matter Hyperintensities
The findings indicated an association between increased WMHV in the whole brain and more frequent physiologically assessed VMS. Upon separate assessments of VMS while asleep and while awake, the association between VMS and whole brain WMHV was strongest for VMS during sleep. These associations persisted despite adjustments for CVD risk factors, demographic variables, and other covariates.
Vasomotor Symptoms and Regional Brain White Matter Hyperintensities
Sleep VMS, in particular, was associated with greater periventricular and deep WMHV. In the context of specific brain regions, there was a consistent association between VMS and WMHV in the frontal lobe, which was evident in VMS while awake and while asleep over a 24-hour period.
Association Between Sleep Vasomotor Symptoms and White Matter Hyperintensities
The association between WMHV and VMS during sleep was consistent even after adjusting for wake-after-sleep onset (WASO) and other covariates. Alteration in the associations of VMS with regional and whole brain WMHV can be explained by the APOE*4 allele carrier status of the study participants; however, there was no significant effect modification. Moreover, there was no association between WMHV and self-reported VMS.
The study concluded that greater WMHV in the whole brain was associated with VMS, with the strongest association for VMS during sleep. VMS can serve as potential markers for brain health in midlife women.
Source
Thurston, R. C., Wu, M., Chang, Y., Aizenstein, H. J., Derby, C. A., Barinas-Mitchell, E., & Maki, P. (2022). Menopausal vasomotor symptoms and white matter hyperintensities in midlife women. Neurology, 100(2), e133–e141. https://doi.org/10.1212/wnl.0000000000201401